
What are Complex Drug Products and Why Should You Care?
Table of Contents
In the past, “complex” drug products simply referred to uncommon products that weren’t your typical tablet. However, with the rise of insoluble APIs, biologics, and 505(b)2 applications, complex dosage forms are quickly becoming the norm. And with this trend, the definition of complex drug products has been broadened to include dosage forms that for one reason or another present an atypical challenge in either manufacturing and/or administration.
In fact, complex drug products have become so prevalent that the FDA has defined them with the following categories:
- Products with complex active ingredients (e.g., peptides, polymeric compounds, complex mixtures of [active pharmaceutical ingredients]); complex formulations (e.g., liposomes, colloids); complex routes of delivery (e.g., locally acting drugs, complex ophthalmological products and otic dosage forms that are formulated as suspensions, emulsions, or gels); or complex dosage forms (e.g., implantables, transdermals, metered dose inhalers, extended-release injectables
- Complex drug-device combination products (e.g., auto-injectors)
- Other products where complexity or uncertainty concerning the approval pathway or possible alternative approach would benefit from early scientific engagement.
While complex products are gaining popularity and there are hundreds of advanced delivery platforms in development, only a handful of technologies are of practical use at this time. Product technology examples in this sector include nanoparticles, drug-eluting systems/devices, liposomes, polymeric microparticles, and so forth. Complex processing challenges include, among others, aseptic manufacturing, the inclusion of highly potent compounds, milling/particle engineering, spray drying, extrusion, and microfluidization.
The Rise of Complex Drug Products
So what has led to this increase in complex drug products? Generally speaking, there are two main drivers:

- Challenging new APIs: Newer therapeutics are frequently not amenable to simple approaches, such as traditional solid oral dosage forms. For small molecules, this is usually related to bioavailability – the API is not soluble and/or has low permeability. Various complex approaches can address this issue. For example, a typical BCS Class II small molecule’s oral bioavailability can usually be substantially increased by reducing particle size. For large molecules, bioavailability (oral) concerns are often accompanied by stability and microbial contamination issues. As a result, these products must be injected and require sterile processing, which adds to the complexity of manufacturing.
- More 505(b)(2) Products: In 2017, there were 63 drug product approvals that used the 505(b)(2) regulatory pathway—an all-time high. This route of approval has become increasingly popular over the last decade and usually involves innovative dosage forms or drug delivery methods that are considered complex. These approaches can greatly improve convenience, economics, and even efficacy. In addition, intellectual property can be gained or circumvented using this approach. As an example, long-acting depot injections have been developed for indications ranging from anti-virals to CNS indications to contraception. These long-acting products drastically increase compliance, improve patient outcomes, and provide additional economic opportunities for their sponsors, but they are considered complex drug products due to the following:
- Challenges in scale-up
- Less defined regulatory pathway
- Complex formulation and excipients
- Complicated characterizations
- No standard in vitro drug release assay
- Few models correlating in vitro drug release with in vivo pharmacokinetics
The Four Categories of Complex Drug Products
In considering the above, complex drug products encompass a wide range of technologies and dosage forms. However, at Particle Sciences, we’ve found that these complex products generally revolve around four conversations or categories:
- Solubilization & Bioavailability Enhancement Techniques
- Drug-Eluting Systems
- Sterile Products
- Highly Potent APIs and/or Controlled Substances
Solubilization & Bioavailability Enhancement Techniques
Why Use Them? Poor water solubility is an increasingly common issue in pharmaceutical development. About 40% of marketed drugs and as many as 90% of drugs in the discovery pipeline are poorly water-soluble. When these drugs are introduced through traditional dosage forms (such as oral solid dose) they fail to dissolve and have limited bioavailability. As a result, insoluble drugs delivered through conventional forms have limited therapeutic effect and often fail. Though not as straightforward, there are multiple techniques available to increase the solubility of drugs and improve their delivery.
“About 40% of marketed drugs and as many as 90% of drugs in the discovery pipeline are poorly water-soluble.”
What Are They?
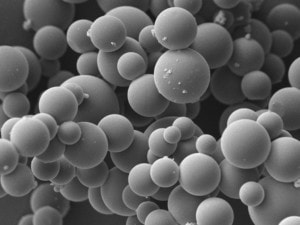
- Particle Size Reduction: Micronization and nanomilling are processes by which a drug is milled or ground down to decrease particle size. As the particle size decreases, the surface area-to-volume ratio increases. This allows for greater interaction with water, which improves solubility and dissolution rate. Particle size reduction is an efficient, reproducible process that allows large quantities of drug to be solubilized at once.
- Amorphous Solid Dispersions: For some drugs, poor solubility is a direct result of a stable crystalline form that water cannot efficiently penetrate. The amorphous form of drug is often more soluble because less energy is required for dissolution. As a result, solid dispersions were developed that distribute the drug in a carrier polymer such as HPMC, preventing it from crystallizing. These amorphous solid dispersions can be produced via hot melt extrusion (HME) or spray drying (SD) processes.
- Encapsulation Techniques: There are a wide variety of encapsulation technologies used in drug delivery, including lipid- and polymer-based systems. And the use of particle-based formulations allows drugs to be encapsulated in a highly soluble form. These technologies offer many attractive attributes for drug delivery, including improved bioavailability, delivery of high doses, protection of the drug from harsh environments, targeted biodistribution of drug, and sustained release of therapeutics. The underlying technologies behind most encapsulated products include: polymeric (PLGA) particles, solid lipid particles, liposomes, and reverse cubic phase particles. Over fifty of these drug products have been approved by the FDA and many more are in clinical development.
- Other Solubilization Techniques: In addition to the above techniques, there are other methods to solubilize drugs, usually involving some combination of pH modification, salt forms, co-solvent systems, surfactants, or complexation with an excipient like cyclodextrin (depending on the physicochemical properties of the API).
What Makes Them Complex? As you can see, many of these techniques require specialized equipment and/or the use of novel excipients to overcome solubility challenges. It is critical to have experience formulating and processing these form factors to understand these uncommon drug-excipient interactions and to have the unique analytical expertise to investigate properties such as particle size or encapsulation efficiency.
Drug-Eluting Systems

Why Use Them? Implantable drug-eluting systems (e.g. combination products, implantable devices, and depot injections) offer several unique advantages over conventional oral or parenteral drug delivery methods. For instance, they can provide localized, site-specific drug delivery, improving the effectiveness of treatment and minimizing side effects. Drug-eluting systems can also be tailored to provide extended release of a drug. These long-acting dosage forms can improve patient compliance because they require fewer doctor visits and dosages than traditional therapies.
What Are They?
Drug-eluting systems are combinations of drug and polymer wherein the polymer acts as a vehicle to deliver the drug. There are two categories of drug-eluting systems: biodegradable and biodurable.
Biodegradable drug-eluting systems (also referred to as bioabsorbable) use biocompatible materials such as Poly Lactic-co-Glycolic Acid (PLGA) to deliver drugs decompose in the body over time. Examples of biodegradable drug-eluting systems include:
- Ozurdex®, a PLGA- dexamethasone rod implanted in the eye to reduce inflammation
- Lupron Depot®, a 1-3 month injection of PLGA microspheres releasing leuprolide acetate for the treatment of advanced prostate cancer in men and endometriosis and fibroids in women
- Biodegradable drug-eluting stents for next-generation angioplasty
Biodurable drug-eluting devices use biocompatible materials like silicone (polydimethylsiloxane or PDMS), polyethylene-vinyl acetate (EVA), and thermoplastic polyurethane (TPU) to deliver drugs. Biodurable drug-eluting devices can be designed as matrix, reservoir, or osmotic systems to deliver drugs via diffusion or osmosis. A commercial example is Merck & Co.’s NuvaRing® EVA intravaginal ring (IVR) that delivers etonogestrel and ethinyl estradiol over 3 weeks. Other examples of biodurable drug-eluting systems include subcutaneous implants, osmotic pumps, and refillable ophthalmic implants.
What Makes Them Complex? The function of drug-eluting systems is heavily dependent on drug-polymer interactions, so polymer selection is a critical part of the formulation process. The selected polymer or polymer blend must provide the desired release profile, drug stability, and compatibility for the application. Additional analytical methods must often be developed to assess drug content, state, and uniformity within a polymer. Drug-eluting systems also employ unique routes of administration; therefore, drug release must be modeled differently than traditional dosage forms like oral or parenteral. And since device manufacturing through HME or injection molding often involves elevated temperatures, the thermal stability of the drug in the polymer must be determined early on. The complexity of drug-eluting systems stems from these unique considerations that follow throughout the formulation process.
Sterile Products
Why Use Them? The FDA requires certain types of drug products to be provided as a sterile dosage forms to avoid the possibility of microbial degradation or infection occurring because of their use. This includes several types of drug products, including injectables (small or large volume parenteral products), ophthalmic drugs, otic dosage forms, and implantable products.
What Are They? Sterility of finished dosage forms can be assured via different processes—either terminal sterilization or aseptic manufacturing.
- Terminal Sterilization: The terminal sterilization process usually involves filling and sealing product containers under high quality environmental conditions designed to minimize microbial and particulate contamination of the product. This minimization of upstream bioburden (the number of microorganisms on a surface) reduces the challenge to the subsequent sterilization. The product is then subjected to a validated sterilization process (e.g. moist heat, irradiation, chemical treatment) in its final container.
- Aseptic Manufacturing: Products that cannot be terminally sterilized due to factors such as API degradation must be aseptically manufactured. Aseptic processing presents a higher risk of microbial contamination than terminal sterilization. In an aseptic filling process, the drug product, containers and closures are sterilized separately and then brought together under an extremely high quality environmental condition designed to reduce the possibility of a non-sterile unit. Any manual or mechanical manipulation of the sterilized drug, containers, or closures prior to or during aseptic filling and assembly poses the risk of microbial contamination.
What Makes Them Complex? The manufacture of sterile products is subject to special requirements in order to minimize risks of microbiological, particulate, and pyrogen contamination. Much depends on the skill, training, and attitudes of the personnel involved. Quality Assurance is particularly important, and sterile product manufacturers must follow established and validated methods of preparation and procedure. Here are just some of the requirements that must be accounted for during sterile operations:

- Cleanroom Architecture – Cleanrooms are rooms designed, maintained, and controlled to prevent particle and microbiological contamination of drug products. Air cleanliness in cleanrooms is maintained using tools like High Efficiency Particulate Air (HEPA) filters, room pressurization sequences, and air change rates. For handling of sterile products, critical areas (ISO 5, Grade A) must be identified to provide the highest level of control to maintain sterility.
- Air Filtration – In addition to the HEPA filters used in cleanrooms, there are many other filtration mechanisms to remove particles from gases and liquids used in pharmaceutical manufacturing. These filters are essential for providing effective contamination control.
- Equipment – To maintain sterility of finished dosage forms, equipment used during manufacturing, filling, and/or packaging must be identified and qualified for the intended purpose. It is important to select equipment which can be sanitized and/or sterilized prior to use to minimize potential microbiological contamination. These processes must be validated as part of the overall sterilization validation strategy.
- Personnel – Personnel pose the greatest risk to the sterility of finished dosage forms. As operator activities increase, the risk to finished product sterility also increases. To ensure product sterility, it is critical for operators to use proper aseptic technique at all times and employ proper application and use of cleanroom gowning materials.
Highly Potent APIs & Controlled Substances
Why Use Them? Many new drugs, especially those for use in cancer treatment, are considered highly potent APIs (HPAPIs). These drugs produce an effect on the body even at low concentrations. Because of this, HPAPIs enable effective treatment with lower doses than traditional drugs.
Controlled substances such as opioids have high addiction potential and require strict documentation and interaction with the DEA. However, many of these drugs are essential for treating conditions such as acute pain or CNS disorders.
What Are They? Potent compounds are typically categorized based on therapeutic class and an acceptable daily exposure limit (ADE), a dose that is unlikely to cause an adverse effect if an individual is exposed, by any route, at or below this dose every day for a lifetime.
The controlled substances list is regulated by the Controlled Substances Act and enforced by the United States DEA. The list is divided into five schedules. Substances are placed in their respective schedules based on whether they have a currently accepted medical use in treatment in the United States, their relative abuse potential, and their likelihood of causing dependence when abused. Schedule I controlled substances have no currently accepted medical use in the United States, a lack of accepted safety for use under medical supervision, and a high potential for abuse. Most pharmaceutically relevant substances fall into schedules II-V. Examples of schedule II drugs include fentanyl, amphetamine, and pentobarbital. Schedule V drugs often contain limited quantities of certain narcotics, like a cough preparation containing a low dose of codeine.
What Makes Them Complex? Both classes of compounds come with increased risk profiles and require extra paperwork and enhanced containment. Working with HPAPIs requires proper safety preparation/planning, facilities to minimize exposure, and personnel who can follow proper protocols. Before an HPAPI is introduced to a facility, a thorough literature search on hazards and a handling strategy must be completed. Monitoring methods for the HPAPIs must then be established, and actual handling of the HPAPI may require specialized PPE and equipment, such as an isolator that separates the compound from the greater environment.

Operations involving controlled substances require many authorizations, licenses, quotas, and levels of security that don’t accompany typical drugs. There are facility requirements, including physical systems to shield controlled substances from the external environment. Employees are also subjected to regular scrutiny from the DEA, who can audit a facility and its operations at any point to maintain licenses to manufacture, store, and distribute controlled drugs.
There are similarities in the level of preparation and protocols that are required for HPAPI and controlled substance handling. Both necessitate specialized training, planning, and facilities, and in some cases, drugs may even fall into both categories. Any company looking to develop products with these drugs must be willing and able to address the added responsibilities that accompany them.
Conclusion
This is the first entry in the Particle Sciences CDMO Services Blog. In this post, we provided an overview of complex drug products, including definitions and a discussion of the unique expertise that these products demand. In the coming weeks, we will continue exploring complex drug delivery topics, including Solubilization & Bioavailability Enhancement Techniques, Drug-Eluting Systems, Sterile Products, and Highly Potent APIs/Controlled Substances.
Particle Sciences is the leading CDMO for complex drug products from early development through commercial supply. We have a seasoned staff and a purpose-built development and manufacturing space, and we work with a range of clients, including small venture-backed firms, not-for-profits, and the world’s largest pharmaceutical and biotech companies. Contact us today to learn more!
Authors: